Guide and Process for Scalp Micropigmentation (SMP)

Introduction:
When compared to hair transplanting, micro-pigmentation is a non-invasive, safe tattooing process. Thousands of small dots that resemble hair roots are tattooed, flawlessly simulating the appearance of hair follicles.
The goal of Scalp Micropigmentation (SMP), a cosmetic tattoo treatment, is to improve density and mimic the look of natural hair follicles by applying natural pigment with a needle to the scalp's epidermal layer. It helps the patient to develop a new hairline by concealing the scalp's surface region where baldness has already started. (Rassman et al., 2015)

What is SMP?
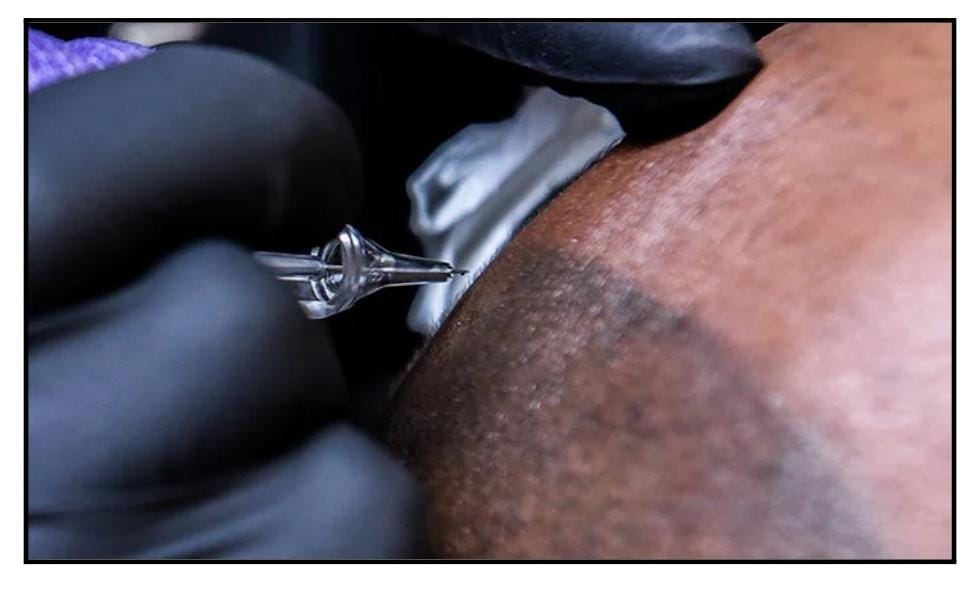
Scalp Micropigmentation, also known as dermopigmentation as well as trichopigmentation, is a type of hair tattooing procedure that involves putting small organic pigments that exactly mimic hair follicles in the top layer of the skin. This dot painting is carried out using a tattoo gun or dermograph, which is furnished with small, disposable needles that are sterilized and contain organic color pigments and pierce the skin at a depth of around 1 millimeter. (Seyhan et al., 2021)
The patient's hair is mimicked by these small colour spots by matching his natural coloring. Depending on the patient's skin type, they can last between three and four years, much like semi-permanent makeup. (Anastassakis, 2023)

The Process Of Scalp Micropigmentation:
The anatomy of the scalp skin is complex. Due to the increased hair thicknesses of terminal hairs, the usual width of the scalp contains a considerable support system for hairs (i.e., glands, nerves, blood vessels, muscles, & fat) in a considerably greater profusion than other locations of body skin.
The big terminal hairs in androgenetic alopecia (AGA) gradually shrink over time as the hair cycles between the catagen and anagen phases. The supporting structure is diminished in proportion to the loss of hair when hair mass is decreased due to miniaturization or apoptosis. (Nguyen et al., 2022)
Candidates For SMP:
- Scarring alopecias on the scalp
- Individuals suffering from autoimmune conditions including refractory
alopecia or alopecia totalis. - Balding or thinning hair in women who are unresponsive to minoxidil or alternative medical therapies and are not candidates for hair transplantation. (Seyhan et al., 2021)
- Scars from head injuries, surgeries, and possibly hair restoration operations as well as scars from neurosurgery.
- Chemotherapy patients who do not get a considerable hair regrowth following treatment
- Deformities in patients undergoing hair restoration due to unanticipated continuous hair loss in males, whose hair transplants did not provide the desired level of "fullness". (Rassman et al., 2015)
- Those who have visible or broad scars from donation strip harvesting methods.
- Patients have open donor scars as a result of strip harvesting operations, that result in punctate scars.
- Patients who have a see-through donor region and/or the classic pluggy or corn-row appearance.
- Those who object to wearing wigs or topical concealers.
- Regional baldness or thinning hair, where the patient wants to seem to have more hair, regardless of shaving the scalp. (Nguyen et al., 2022)
What Is The Procedure For SMP?
- The first step in the SMP procedure is the insertion of a tiny droplet of pigment into the dermis's top layer via the skin using a normal tattoo tool that can accommodate one to six needles revolving between 100 and 150 cycles each second.
- To reach the higher dermis, the needle(s) must pierce the epidermis. The operator's "feel" and visual assessments, which take into account the undulating thicknesses of the dermis at the place of entry, affect how deeply the needle is inserted.
- It will affect how the operator feels and perceives the SMP process since a thicker scalp with extra fat and supporting tissue will provide a different skin momentum than the atrophic or scarred scalp. As the operator continuously modifies the impacts that are felt and observed, a mental feedback loop is created. (Anastassakis, 2023)
- To apply the precise amount of pigment to the scalp at the proper level for the desired result, other considerations become crucial.
- It is often advise to perform several sessions. Each session's amount of "dots" might exceed 40,000 points. The sessions are frequently lengthy, lasting as much as 8 hours each.
- Before moving on to the next stage of the treatment, pigment bleeding will need to be treated in every given session, maybe using a Q-switched laser. (Seyhan et al., 2021)
Colour Shifts:
It is crucial to let the patient know that the pigment may have a blue and green tinge. The red blood veins under the skin look green because of more absorption in the red portion of light, which is a phenomenon that is clarified by the trichromatic concept of colour vision. (Rassman et al., 2015)
This is analogous to the greenish hue of the black or grey pigment. As a result of direct UV light contact on the dye through the skin, some pigments can actually shift in color, which might improve the trichromatic process.
Histology Of Skin Pigments:
- The concentration of pigment that persists throughout the first several days after the pigment has been applied to the scalp reveals its size and depth of application. The epidermis is between 0.5 and 1.5mm thick.
- The principal barriers for the skin's defence are the stratum corneum or stratum granulosum. The stratum spinosum, the thickest layer of the epidermis, fills with colour in the path the needle(s) leaves behind. (Seyhan et al., 2021)
- The stratum basale, the epidermis from the dermis, is the layer of the epidermis that is the thickest. These cells move upward and towards the surface when they are actively mitotic.
Properties Of Skin Pigments:
- While the insoluble pigment components are integrated with the fibrous tissue which surrounds each fibroblast harboring ink particles, some of the soluble pigment components may initially be absorbed and removed by the lymphatic system. (Anastassakis, 2023)
- Washing out of the outermost epidermal pigments and escape (bleeding) of the epidermal pigment outside of the region it was implanted are two alterations that are frequently seen in these initial stages after the procedure has occurred.
- The skilled practitioner must strike a balance between what is visible at the time of the initial operation and the expected loss of some of the most superficial epidermal pigments over a period of time. (Seyhan et al., 2021)
- In the first few days following the operation, some colour leakage might be noticed due to the stratum corneum being breached. Some pigments can get absorbed over time or change colour because the dermal pigment is initially unstable when subjected to the body's response to external bodies. (Nguyen et al., 2022)
How To Prepare For SMP?
- Following the treatment, patients are advised to adhere to specific safety precautions, including a 28-day restriction from using saunas and steam rooms, along with a recommendation to abstain from strenuous physical activity for five days. (Anastassakis, 2023)
Risk Factors Of SMP:
Mycobacterium chelonae infection, allergies to the pigment component causing scarring, granulomas via foreign body reactions, and MRI-induced complications are some of the infections that have been linked to contaminated tattoo inks.
These infections have raised concerns about the sufficiency of packaging, sterilization, use of dirty or recycled needles, and improper techniques across the tattoo parlor level. (Rassman et al., 2015)
Unsterile tattooing supplies and needles have reportedly been shown to spread infectious illnesses such as the human immunodeficiency virus, cirrhosis, and skin infections brought from Staphylococcus aureus along with other pathogens.
Although uncommon, some individuals may experience a reaction of allergy to the ink's pigments. People who are susceptible to keloid scarring might not be good candidates for SMP. After an accident or other skin damage, some people may acquire keloid scars, which are thick, elevated scars. (Seyhan et al., 2021)
There have been a few accounts of tattoos or permanent tattoos giving people a swollen or burning feeling during an MRI scan. People should let a radiologist know in advance even if the danger could be minimal. (Anastassakis, 2023)
Conclusion
Scalp Micropigmentation (SMP) can serve as a viable alternative or complement to hair transplantation. This approach is gaining increasing popularity and has received positive feedback from patients. Fundamental SMP training is essential for healthcare professionals seeking to offer optimal care to individuals seeking to conceal their hair loss.
References
- Rassman, W. R., Pak, J. P., Kim, J., & Estrin, N. F. (2015). Scalp
micropigmentation: a concealer for hair and scalp deformities.
The Journal of Clinical and Aesthetic Dermatology, 8(3), 35.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4382144/ - Seyhan, T., & Kapi, E. (2021). Scalp micropigmentation procedure:
a useful procedure for hair restoration. Journal of Craniofacial
Surgery, 32(3), 1049-1053.
https://journals.lww.com/jcraniofacialsurgery/Fulltext/2021/050
00/Scalp_Micropigmentation_Procedure__A_Useful.56.aspx - Anastassakis, K. (2023). Scalp Micropigmentation. In Androgenetic Alopecia From A to Z: Vol. 3 Hair Restoration Surgery, Alternative Treatments, and Hair Care (pp. 537-555). Cham: Springer International Publishing
https://link.springer.com/chapter/10.1007/978-3-031-10613-2_35 - Nguyen, B., Mervis, J. S., Romanelli, P., & Tosti, A. (2022). Scalp Micropigmentation: A Clinicopathologic Correlation. Skin appendage disorders, 8(5), 412-414.
https://karger.com/sad/article/8/5/412/826775

Company
Need Help?
Recruitment
Made in Europe ©2024 Skillmed